Thursday, May 22, 2008
Plavix (Clopidogrel) associated TTP
An important reminder regarding Plavix.
Clopidogrel (Plavix) is used commonly in patients with cerebrovascular and coronary disease as an antiplatelet drug. Now there are substantial number of cases reported in literature of thrombotic thrombocytopenic purpura (TTP) associated with use of Clopidogrel (Plavix).
Clopidogrel-associated TTP often occurs within 2 weeks of drug initiation and has a high mortality if not treated promptly.
Key is prompt diagnosis as the survival rate for clopidogrel-associated TTP is almost 100% if therapeutic plasma exchange performed within 3 days of onset of TTP (100% vs 27.3%).
References: Click to get abstract if available
1. Clopidogrel-Associated TTP - Stroke. 2004;35:533
2. Clopidogrel and thrombotic thrombocytopenic purpura: No clear case for causality - CLEVELAND CLINIC JOURNAL OF MEDICINE , VOLUME 70 • NUMBER 5, MAY 2003 -pdf file
3. Thrombotic thrombocytopenic purpura associated with clopidogrel administration: case report and brief review. Am J Med Sci 2001; 322:170–172.
4. Plasmapheresis improves survival in drug-induced thrombotic thrombocytopenic purpura: systematic review of published case reports [abstract]. Blood 2001; 98(Suppl 1):60b.
5. Thrombotic thrombocytopenic purpura occurring after exposure to clopidogrel [abstract]. Blood 1999; 94(Suppl 1):78b.
6. Clopidogrel-associated TTP [abstract]. Transfusion 1999; 39(Suppl):56S.
7. Clopidogrel and thrombotic thrombocytopenic purpura. N Engl J Med 2000; 343:1193–1194.
Wednesday, May 21, 2008
Troponin I Elevation in patients without Acute Coronary Syndromes !
Q; How many patients may have Cardiac Troponin I elevation without Acute Coronary Syndromes ?
A; Upto 35% !!
In a recent paper, just published in Am J Cardiol 1, 883 consecutive hospitalized patients were studied with increased cardiac troponin I levels. The discharge diagnosis was reclassified and troponin increase attributed to ACS or another process. Patients were followed for a median of 30 months.
Results: 311 patients were classified as having a non-ACS–related troponin increase (35.2%). An alternative explanation for troponin increase was found in 99% of these patients. Troponin level had poor accuracy in discriminating patients with and without ACS.
Of the 311 patients without ACS,
- 89 (28%) were diagnosed as having sepsis,
- 49 (16%) had acute left heart failure,
- 41 (13%) were after coronary artery bypass graft,
- 31 (10%) had atrial or ventricular arrhythmia,
- 23 (7%) were after cardiopulmonary resuscitation,
- 21 (7%) had a cerebrovascular event,
- 11 (4%) had myocarditis,
- 11 (4%) had acute bleeding,
- 10 (3%) had chest contusion,
- 6 (2%) had pulmonary embolism.
- 19 patients (6%) had another diagnosis such as diabetic ketoacidosis, carbon monoxide intoxication, pancreatitis, hypoxemia, hypercarbia, lymphoma, and electrocution.
Mean serum troponin level for
- patients without ACS were significantly lower (15.3 +/- 15.9 ng/ml)
- the values of patients with STEMI (32.5 +/- 18.1 ng/ml)
- NSTEMI (20.4 +/- 18.4 ng/ml)
- The highest troponin level in the non-ACS group was found in 10 patients diagnosed as having myocarditis (27.7 +/- 21.5 ng/ml)
Coronary angiography was frequently unhelpful in excluding a non-ACS–related troponin increase because 77% of patients in the non-ACS group had significant flow-limiting coronary artery disease.
But patients with non-ACS–related troponin increase had significantly higher in-hospital and long-term mortalities compared with patients with ACS.
Conclusion:
Cardiac Troponin I Elevation in Hospitalized Patients Without Acute Coronary Syndromes - Am J Cardiol 2008;101:1384–1388, 15 May 2008
Tuesday, May 20, 2008
Tuesday May 20, 2008
Acute Liver Failure
Q; The chances of survival with medical management in acute liver failure is 26%. How much difference liver transplant can make?
A; It goes upto 90% !!
Watch video lecture
Acute Liver Failure: The Critical Team Approach *
Dr. Lorenzo Rossaro, Chief of Gastroenterology and Hepatology and Head of the Liver Transplant Program at University of California Davis Medical Center.
*Total time: 42 minutes. Please click on above link. You need Real Player to watch the lecture
Monday, May 19, 2008
Hydrocortisone in septic shock - controversy continues
Controversy over use of Hydrocortisone in septic shock has been hot particularly after recent publication and criticism of CORTICUS trial. Just few days ago, we posted a concise commentary on this issue from Dr. Jean-Louis Vincent (here). One very recent study (from Annane group) now looked into relationship between cardiovascular autonomic modulation and adrenal function during sepsis.
Patients and Method: Cardiovascular variability was assessed by spectral analysis of heart rate and diastolic blood pressure signals, which included computation of normalized low (LFnu) and high frequency (HFnu) components.
In study phase 1, the spectral analysis of heart rate and diastolic blood pressure was obtained in five septic shock and six healthy volunteers before and 60 min after a single intravenous bolus of 50 mg of hydrocortisone.
In study phase 2, the spectral analysis of heart rate and diastolic blood pressure was obtained in 47 consecutive patients with septic shock immediately before a 250 μg adrenocarticotropic hormone (ACTH) stimulation test and before initiation of corticosteroids. Spectral components were compared between patients with adrenal insufficiency and those with presumed normal adrenal function. Adrenal insufficiency was defined as a basal cortisol of less than 15 μg/dl or a maximal cortisol increment after 250 μg of ACTH of less than 9 μg/dl.
Study phase 3 focused on 23 consecutive patients with septic shock and adrenal insufficiency. Spectral components were obtained immediately before and at day 3 after initiation of 50 mg every 6 hrs of hydrocortisone and 50 μg daily of fludrocortisone, or their respective placebos in a double blind manner.
Results:
- As compared to healthy volunteers, patients had decreased LFnu-HR and LFnu-DBP and, after hydrocortisone, they had a greater increase in LFnu-DBP (p = .01)
- As compared to patients with normal adrenal function, those with adrenal failure had decreased LFnu-HR and LFnu-DBP
- In patients with adrenal failure, as compared to placebos, hydrocortisone plus fludrocortisone increased significantly LFnu-DBP (p = .02) and low frequency/high volume ratio (p = .009)
Conclusion: In septic shock, the loss in cardiovascular variability is more marked in patients with adrenal insufficiency and is partly restored by exogenous administration of corticosteroids.
Reference: click to get abstract
Hydrocortisone effects on cardiovascular variability in septic shock: A spectral analysis approach - Critical Care Medicine. 36(5):1481-1486, May 2008.
Sunday, May 18, 2008
Case: 58 year old male with history of "CHF" presents to ER with shortness of breath. On exam patient appear to have classic signs of 'exacerbation of CHF'. Patient also complain of nausea, vomiting, diarrhea and abdominal pain. Also, patient sees everything green, double and blurred ! Labs are not back yet but following EKG is obtained. With above history, what is your suspicion ?
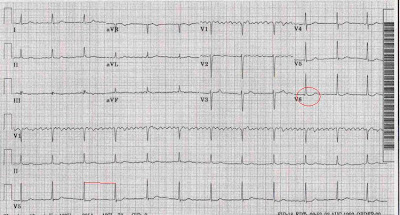
Answer: Digoxin Toxicity
The 3 major hallmarks on EKG of Digoxin toxicity
- accelerated junctional rhythm, also called "regularized Atrial Fibrillation"
- ST segment sagging (This finding is not indicative of toxicity unless other signs present)
- a shortened QT interval
First rule is - Comparison with previous EKGs.
Many times, its hard to find any specific EKG sign. Digoxin toxicity may cause any dysrhythmia including paroxysmal atrial tachycardia with 2:1 block, accelerated junctional rhythm, or even torsade de pointes. Premature ventricular contractions (PVCs) are very common. Bigeminy or trigeminy can be seen frequently. Sinus bradycardia, other bradyarrhythmias, First- and second-degree AV block, complete AV dissociation, and third-degree heart block are very common too.
Cardiac arrest - Ventricular tachycardia,asystole, ventricular fibrillation - is hard to rescue and usually fatal.
Saturday, May 17, 2008
Diastolic Blood Pressure: A Reliable Early Predictor of Survival in Human Septic Shock !
Very interesting article published this month 1. A must read !!
Background: Emphasis in therapy of human septic shock is shifting towards reliable end points and predictors of survival. Rationale is to study whether the evolution of cardiovascular reactivity in view of the administered doses of norepinephrine is an early predictor of inhospital survival and to determine the optimal threshold of norepinephrine therapy and its consequences on renal function.
Methods: Observational study of a prospective cohort of patients in septic shock, hospitalized in ICU least 24 hours before requiring norepinephrine.
Excluded were patients requiring less than 72 hours of continuous norepinephrine (16 patients) or who received corticosteroids.
Hemodynamic parameters (heart rate, blood pressure, urinary output, and temperature) were continuously monitored.
Results: Of 68 patients, 45 survived ICU stay of 24 (12–36) days, hospital stay of 36 (27– 66) days], and 23 died 5 (3–10) days after septic shock onset and norepinephrine treatment.
Multivariate analysis revealed four independent positive predictive factors of short-term (10 days) outcome:
- Simplified Acute Physiology Score (SAPS) II less than 50
- on day 3 Logistic Organ Dysfunction System (LODS) score less than 6
- norepinephrine concentration less than 0.5 g/kg/min
- diastolic arterial pressure >50 mm Hg, but not systolic arterial pressure
Conclusions: Septic shock survival increases when dose of 0.5 g/kg/min of norepinephrine continuously improves vascular tone within the first 48 hours, or when diastolic arterial pressure (>50 mm Hg) is restored. Norepinephrine has beneficial effects on renal function. Predictive value of LODS score on day 3 is demonstrated, while SAPS II is confirmed as the only reliable predictive factor in first 24 hours.
Pearl contributed by
Anthony Halat, M.D.
ICU Physician, Medical ICU,
The Methodist Hospital,
Texas Medical Center, Houston, TX
Reference: click to get abstract
Diastolic Arterial Blood Pressure: A Reliable Early Predictor of Survival in Human Septic Shock. - Journal of Trauma-Injury Infection & Critical Care. 64(5):1188-1195, May 2008.
Friday, May 16, 2008
Q: 52 year old male, who recently travelled, having charity work at rural africa, presented with shortness of breath. Following CXR was obtained. On examination, patient noticed to have 'painless' ucerated lesions over skin.


With travel history, widened mediastinum and ulcerated cutaneous ulcer. What is your biggest concern?
A; Anthrax
Anthrax is primarily a disease of livestock, such as sheep, cattle, or goats, and most cases occur in developing countries. But lately it found fame as a potential agent of bio-terrorism.
Progressive widened mediastinum is one hallmark of anthrax infection. Inhalational anthrax presents as hemorrhagic mediastinitis, not pneumonia, which may be associated with bloody pleural effusions.
Cutaneous anthrax (skin manifestation) is most common and begins as a pruritic papule that enlarges in 24-48 hours to form an ulcer surrounded by edematous halo. The cutaneous anthrax ulcer is usually pruritic but not painful.
Penicillin, Doxycycline or any Quinolone is the treatment.
See concise ppt presentation on Anthrax here (from Suzanne R. White, M.D., Departments of Emergency Medicine & Pediatrics, Wayne State University, Detroit Medical Center, Michigan)
Thursday, May 15, 2008
Intensivist !
Studies after studies have suggested that quality of care in hospital ICUs is strongly influenced by whether intensivists are providing care and the staff organization in the ICU. Mortality rates are significantly lower in hospitals with ICUs managed exclusively by board-certified intensivists. Research has shown that in ICUs where intensivists manage or co-manage all patients versus low intensity there is a 30% reduction in hospital mortality and a 40% reduction in ICU mortality.
If you need to talk to hospital administration ! and for more information on Leapfrog’s ICU Physician Staffing requirements, click on below links and keep in file (pdf documents).
Leapfrog’s ICU Physician Staffing requirements (updated April '08)
Leapfrog’s ICU Physician Staffing Bibliography (33 references - updated Feb. 2008)

Wednesday, May 14, 2008
BNP to predict weaning from ventilator?
Very interesting observation !
Introduction: Despite the use of spontaneous breathing trial (SBT), predicting weaning success remains a major clinical challenge. Because cardiovascular dysfunction could be a major underlying mechanism of weaning failure, role of the levels of B-type natriuretic peptide (BNP), a marker for cardiovascular function, was evaluated in patients who passed a 2 hour SBT.
Design, Setting, and Patients: It was a 3 step study, First: 52 patients recovering from acute respiratory failure were enrolled as the testing group to determine the predictive value of BNP. Second: The predictive value of BNP was validated in a second independent cohort of 49 patients. Third: Both groups of patients were combined to conduct the final analysis.
Measurements and Results:
In the testing group of 52 patients, 41 passed SBT and were extubated. Of these patients, 33 patients (80%) were extubated successfully (extubation success) while eight patients (20%) were reintubated within 48 hrs (extubation failure). There were no differences in the baseline BNP levels, but the extubation failure group had significantly greater increases in BNP at the end of SBT than the extubation success groups
An increase of BNP less than 20% during SBT had the best combination of sensitivity, specificity, positive and negative predictive values, and diagnostic accuracy for predicting extubation success (91%, 88%, 97%, 70%, and 91%).
Combining BNP with SBT as extubation criteria increased the extubation success rate to 95% from 78% using SBT alone (p = .035).
Conclusion: Measuring the percentage change in the BNP level during a SBT may help improve the predictive value of SBT on weaning outcome.
Reference: click to get abstract
Changes in B-type natriuretic peptide improve weaning outcome predicted by spontaneous breathing trial - Critical Care Medicine. 36(5):1421-1426, May 2008.
Tuesday, May 13, 2008
Adrenal insufficiency in prolonged critical illness
Interesting work from Taiwan !
Introduction: Adrenal insufficiency is frequently found in critically ill patients and affects their prognosis. But little is known about how the adrenal function changes during prolonged critical illness. This study was conducted to investigate the dynamic changes of cortisol levels in patients with critical illness who do not improve after treatment.
Methods: This observational cohort study was performed in the intensive care units of a university hospital. Acutely ill patients with initial cortisol level above 34mug/dL but without improvement after treatment, and who had follow-up cortisol levels during their critical illness, were studied. All clinical information and outcomes were recorded.
Results: 53 patients (with initial cortisol level above 34mug/dL) were included.
- 10 patients had follow-up cortisol levels remained more than 34mug/dL,
- 32 patients between 34 and 15mug/dL, and
- 15 patients less than 15mug/dL
Outcomes did not differ significantly among the three groups with different second cortisol levels.
In Cox regression analysis, patients who survived to hospital discharge with second cortisol levels less than 15mug/dL had a longer hospital length of stay (p = 0.004).
Conclusion: The majority of acutely ill patients who remained in critical condition had decreased serum cortisol levels. Lower follow-up cortisol levels might lead to worse clinical outcomes. Repeated testing for adrenal function is suggested for patients with prolonged critical illness.
Reference: click to get abstract
Adrenal insufficiency in prolonged critical illness: Critical Care 2008, 12:R65
Monday, May 12, 2008
On Zosyn's (Piperacillin/tazobactam) dose in nosocomial and ventilator-associated pneumonia
Does Piperacillin/tazobactam (Zosyn) reaches adequate alveolar concentration (as needed in nosocomial and ventilator-associated pneumonia) at any dose of continuous infusion? Recent study by Emmanuel helped to address this issue.
Patients: 40 patients with microbiologically documented ventilator-associated pneumonia (VAP).
Interventions: Patients were randomized to receive piperacillin/tazobactam daily continuous infusions of
- 12/1.5 g/day or
- 16/2 g/day after a loading dose of 4/0.5 g
Conclusions: A target piperacillin serum concentration of at least 35-40 mg/L is probably required to provide alveolar concentrations exceeding the susceptibility breakpoint for Gram-negative bacteria (16 mg/L) during ventilator-associated pneumonia.
In patients with no/mild renal failure, a continuous daily dose of piperacillin/tazobactam 16/2 g/day allows reaching this target concentration, which might be not observed with 12/1.5 g/day.
In patients with moderate/advanced renal failure, both dosages achieve serum concentrations far above the 35-40 mg/L threshold, suggesting that in that case, therapeutic drug monitoring should be performed in order to adjust the daily dose.
Editors' comment: Zosyn is a frequent antibiotic used for Nosocomial and VAP(Ventilator associated Pneumonia) in USA but mostly in divided doses, instead of continuous infusion (as this study was done in France). This study translates into conclusion that patients with no renal insufficiency requires higher dose of Zosyn to treat Nosocomial and VAP (around 4.5 q 6 hours). But patients with renal insufficiency needs lower dose and drug monitoring is recommended.
reference: click to get abstract
Boselli E, Brelith D, Rimmele T, Guillaume C, Xuereb F, Saux MC, et al. Alveolar concentrations of piperacillin/tazobactam administered in continuous infusion to patients with ventilator-associated pneumonia. Critical Care Medicine. 36(5):1500-1506, May 2008.
Sunday, May 11, 2008
Revisiting basic
Q: According to landmark expert panel conference of 1991/1992, under the auspices of the American College of Chest Physicians and the Society of Critical Care Medicine, what is the widely accepted definition of SIRS (Systemic inflammatory response syndrome) ?
A: SIRS is defined as 2 or more of the following variables:
- Fever of more than 38°C ( 100.4°F) or less than 36°C ( 96.8°F)
- Heart rate of more than 90 beats per minute
- Respiratory rate of more than 20 breaths per minute or a PaCO2 level of less than 32 mm Hg
- Abnormal white blood cell count (>12,000/µL or <4,000/µl>>10% bands)
Reference:
Bone RC, Balk RA, Cerra FB, et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Chest. 1992;101:1656-1662
Saturday, May 10, 2008
Perfusion site
Comprehensive site for anyone interested to learn and to have resource link available in cardiac anaesthesia and cardiopulmonary bypass.
http://www.perfusion.com.au/CCP/ccp_notes.htm
(Page of Australian & New Zealand College of Perfusionists)
Friday, May 9, 2008
Bedside tip - Changing cordis to tripple lumen
This is a regular practice to change cordis (large bore or rapid infuser catheter) to (small bore) central line "over wire", once need for cordis itself is over (like removal of pulmonary artery catheter or need of rapid fluid infusion).
One frequent issue is inability to advance wire in cordis. As cordis is large bore, its 'hub' (see picture below) tends to bend at skin or inside sucutaneous tissue, which prevents advancement of wire. Trick is to retract the cordis about 1-2 cm out of skin, make it straight and advance wire.
Proceed further with usual practice of changing catheters over wire.
Previous related pearls:
Peres Nomogram to calculate required length of central line
Bedside tip - central line removal
Suture at central venous catheter site - a risk ?
Appropriate length of guide wire to advance
Thursday, May 8, 2008
ECMO update
Extracorporeal membrane oxygenation (ECMO) refers to the technique of providing both cardiac and respiratory support oxygen to patients by draining blood from the venous system and oxygenating it outside of the body. ECMO uses cardio-pulmonary bypass technology to temporarily provide gas exchange to patients with severe, but potentially reversible, respiratory failure. ECMO is a standard practice in neonatal and pediatric ICUs to support pulmonary failure but remained a very last resort in adult ICUs due to the high technical demands, cost, and risk of bleeding (requires anticoagulation). The major reason ECMO remained unused in adult ICUs is a negative study done about 29 years ago. The National Institutes of Health trial of ECMO in severe acute respiratory failure in 1979 showed mortality in excess of 90% .
ECMO could be a bridge till definite therapy is sought or till healing occurs. Technically, VV or VA (veno-veno or veno-arterial) ECMO can provide sufficient oxygenation for several weeks.
One recent trial called CESAR (Conventional Ventilation or ECMO for Severe Adult Respiratory Failure) showed increase survival among adult patients with severe but potentially reversible respiratory failure compared with conventional ventilatory support.
Data from CESAR trial showed that ECMO may increase the rate of survival without severe disability 6 months after randomization and may be cost-effective compared with conventional ventilatory support.
The conventional treatment group was treated with standard clinical practice, with a low-volume ventilation strategy.
The primary outcome measure was death or severe disability 6 months after randomization and included deaths before hospital discharge if occurring after 6 months.
Severe disability was defined as being both "confined to bed" and "unable to wash or dress oneself."
Patients: A total of 180 patients from 68 centers were randomly assigned to receive
- conventional ventilation (n = 90)
- ECMO (n = 90)
Of the 90 patients assigned to receive ECMO, 22 did not receive ECMO, most often because they improved without it.
A significant number of patients had failure of more than 3 organs in both groups (28 in the ECMO group and 27 in the conventional group).
Results:
- Of the patients randomly assigned to receive ECMO, 57 of 90 met the primary endpoint of survival or absence of severe disability at 6 months compared with 41 of 87 evaluable patients in the conventional ventilation group (survival benefit 63% vs 47%).
Conclusion: The benefit of ECMO was seen regardless of several factors including hospital of trial entry, age, presence of hypoxia, duration of high-pressure ventilation, primary diagnosis at trial entry, and number of organs failed.
Initial data presented by Giles J. Peek, MD, FRCS, from the University of Leicester, Glenfield, United Kingdom, at the Society of Critical Care Medicine 37th Critical Care Congress 2008, Hawaii.
Pre-report details can be read
Wednesday, May 7, 2008
Nebivolol (Bystolic)
Q: How nebivolol (Bystolic), the newly approved beta-blocker, is different from previously approved 18 other beta-blockers?
A: Nebivolol is said to be the 19th beta blocker approved for US market. Nebivolol (Bystolic), is approved by FDA for the treatment of hypertension. The drug is a selective beta 1 blocker but has the added pharmacological properties of producing vasodilation and reducing total peripheral resistance brought about by modulation of nitric-oxide release, rather any receptor blockade.
Coreg (Carvedilol) is another new generation b-blocker which does vasoldilation, but via alpha receptor blocakade.
Because of vasodilatory properties Nebivolol and Coreg have also shown benefit (vs placebo) in heart failure. Unlike Coreg, Nebivolol is not approved for the treatment of heart failure (yet).
Previous related pearls: Regarding Coreg
Monday, May 5, 2008
Q: What is the drug of choice to control cocaine induced seizures?
A: Diazepam and lorazepam.
Also, barbiturates, may be effective in controlling seizures because they may act synergistically with the benzodiazepines.
Important pearl to remember is: Phenytoin may not be effective against cocaine-induced seizures.
Sunday, May 4, 2008
Q: What is the ratio of alpha and beta blockade in Labetalol?
A: As an anti-hypertensive, Labetalol has both alpha-blockade and beta-blockade activity. The ratio of alpha to beta blockade activity is
1:3 when used Orally
1:7 when used intravenously
References:
1. I.V. LABETALOL AND CORONARY ARTERY SURGERY, MOREL et al. Br. J. Anaesth..1984; 56: 664-665
2. Comparative study of esmolol and labetalol to attenuate haemodynamic responses after electroconvulsive therapy - Kathmandu University Medical Journal (2007), Vol. 5, No. 3, Issue 19, 318-323, pdf file
Saturday, May 3, 2008
Steroids in sepsis controversy - what 'Guru' thinks !
Here is a very well rounded commentary on steroids in sepsis from internationally famed Critical Care master Dr. Jean-Louis Vincent. We are just posting important points from commentary due to space constrain. You can read full text with references by clicking at link below:
"............Forty years ago, high-dose steroids were used in the belief that, because sepsis is an inflammatory response, the anti-inflammatory properties of steroids could be useful. Initial studies were encouraging, with Schumer demonstrating that treatment with one or two doses of intravenous dexamethasone (3 mg/kg) or methylprednisolone (30 mg/kg) was associated with reduced mortality compared with saline treatment in patients with septic shock. Two large, double-blind, randomized controlled trials later failed to confirm these findings, however, and two meta-analyses in the mid 1990s concluded that steroids were ineffective or indeed were potentially harmful in sepsis.
Then, in the late 1990s, several studies were published suggesting a role for much smaller, so-called stress, doses of steroids in reducing vasopressor requirements in patients with septic shock. These results led to a study by Annane and colleagues in which patients with relative adrenal insufficiency – as assessed by nonresponse to a corticotropin test – who were treated with hydrocortisone (50 mg intravenously every 6 hours) and fludrocortisone (50 μg orally daily) for 7 days had a reduced mortality compared with nonresponders treated with placebo. Despite concerns regarding the lack of statistical significance in overall mortality rates at 28 days, the results from this study led to steroids being recommended in the treatment of patients with septic shock. Steroid use was also incorporated into the so-called sepsis bundles, with the recommendation that all patients with septic shock should receive low-dose corticosteroids within 24 hours of diagnosis.
Doubts remained, however, and a large, international, multicenter study was conducted to confirm the results of the earlier study. The Corticus – Corticosteroid Therapy of Septic Shock – study, which included close to 500 patients, recently showed that hydrocortisone did not improve survival or reversal of shock in patients with septic shock, either overall or in patients who did not respond to a corticotropin test. The results from the Corticus study were somewhat disappointing, and, in the accompanying editorial, Dr Finfer suggested the need for a further study to explore the effects of steroids in septic shock in a much larger population. With no signal from the Corticus study, however, merely increasing the size of the study is unlikely to show mortality differences.
Importantly, apart from the differences in effects on outcome, there were other notable differences between the Corticus study and Annane and colleagues' study, including the larger number of postoperative patients, the more common abdominal source of the sepsis, and, in particular, the lower severity of illness in the Corticus study. This latter factor is particularly important and can be explained by the fact that many patients with severe septic shock were treated with steroids in accordance with guidelines current at the time of the study, and hence were excluded from enrollment – so the included population, by definition, consisted of less severely ill patients. As a result of this lower severity of illness, the mortality rate in the Corticus study was about one-half that of Annane and colleagues' study. It is therefore still possible that steroids may decrease mortality in very ill patients, just not in those with moderately severe shock.
Similar observations were made with activated protein C, another adjunct therapy for sepsis, which was shown to reduce mortality in very ill patients but not in those patients with a lower risk of death. I believe we do need another trial of steroids in sepsis, but specifically in patients with severe septic shock rather than just in a larger general population of septic shock patients.
...................Perhaps the time has come to take a step back and reflect on past efforts so that future clinical trials will be conducted in an optimal manner to limit the pendulum effect and to provide results that stand up to scrutiny and can be immediately introduced into clinical practice to the benefit of our patients."
Reference: Steroids in sepsis: another swing of the pendulum in our clinical trials, Jean-Louis Vincent, Department of Intensive Care, Université libre de Bruxelles, Erasme Hospital, Brussels, Belgium, Critical Care 2008, 12:141
Friday, May 2, 2008
Digoxin recall !!
A class I recall is being issued on all Digitek (digoxin) tablets, which may contain twice the approved level of digoxin.
Digitek is a registered trademark of Actavis Totowa (formerly Amide Pharmaceutical, Inc.) for their digoxin tablets. The drug is distributed by Mylan Pharmaceuticals Inc., under a “Bertek” label and by UDL Laboratories, Inc. under a “UDL” label.
See FDA press release here
Previous related pearls on "Dig."
Treating Digoxin toxicity 1
Treating Digoxin Toxicity 2
What Dig. level makes you happy?
Adenosine and Digoxin !
Thursday, May 1, 2008
Conivaptan's (Vaprisol) drug interactions
Q: Conivaptan (Vaprisol), a Vasopressin Antagonist, which is indicated for the management of euvolemic hyponatremia - can increase the concentration of following drugs if use concomittently? (choose one)
A) Amlodipine (Norvasc)
B) Simvastatin (Zocor)
C) Digoxin (Lanoxin)
D) Midazolam (Versed)
E) All of the above
Answer is E: All of the above
Administration of oral conivaptan 40 mg twice daily with amlodipine besylate (Norvasc) resulted in a two-fold increase in the AUC concentration and increased half-life of amlodipine.
The combined use of IV conivaptan and midazolam should be avoided, because the AUC concentration of midazolam may be increased by two-fold to three-fold when these agents are used together.
The coadministration of conivaptan and HMG-CoA reductase inhibitors (statins) such as simvastatin (Zocor) should also be avoided because the AUC concentration of the statin is increased by three-fold.
Digoxin when taken with oral conivaptan, results in a 30% reduction in clearance of digoxin.
Read nice review on Conivaptan
(reference: P&T • March 2007 • Vol. 32 No. 3, Page 140)
